উচ্চ ৰক্তচাপ
| উচ্চ ৰক্তচাপ (Hypertension) | |
|---|---|
| অন্য নাম | ধমনীৰ উচ্চ ৰক্তচাপ |
 | |
| উচ্চ ৰক্তচাপ প্ৰদৰ্শন কৰা এটা স্নয়ংক্ৰিয় ৰক্তচাপ যন্ত্ৰ (চিষ্ট'লিক ধমনী চাপ 158 mmHg, ডায়েষ্ট'লিক ধমনী চাপ 99 mmHg আৰু হৃদ কম্পন মিনিটত ৮০ বাৰ।) | |
| বিভাগ | হৃদৰোগ বিভাগ |
| লক্ষণ | নাই[1] |
| জটিলতা | ক'ৰ'নেৰী ধমনী ৰোগ, ষ্ট্ৰ'ক, হাৰ্ট ফেইলাৰ, প্ৰান্তীয় সংবহনতান্ত্ৰিক ৰোগ, অন্ধত্ব, দীৰ্ঘম্যাদী বৃক্কৰ ৰোগ[2][3] |
| কাৰণ | সাধৰণতে জীৱনশৈলী আৰু জিনীয় কাৰক[4][5] |
| ৰোগ নিৰূপণ | বিশ্ৰাম অৱস্থাত ৰক্তচাপ > ১৪০/৯০ mmHg[4] |
| চিকিৎসা | জীৱনশৈলী পৰিৱৰ্তন, ঔষধ[6] |
| পুনৰাবৃত্তি | বিশ্বজুৰি ১৬-৩৭%[4] |
| মৃত্যু | ৯.৪ নিযুত / ১৮% (২০১০)[7] |
উচ্চ ৰক্তচাপ (Hypertension, HTN or HT), এটা দীৰ্ঘম্যাদী ৰোগ য'ত ধমনীৰ ৰক্তচাপ জোখতকৈ বেছি থাকে।[8] উচ্চ ৰক্তচাপৰ সাধাৰণতে কোনো লক্ষণ নাই।[1] দীঘদিনীয়া উচ্চ ৰক্তচাপৰ ফলত ক'ৰ'নেৰী ধমনী ৰোগ, ষ্ট্ৰ'ক, হাৰ্ট ফেইলাৰ, প্ৰান্তীয় সংবহনতান্ত্ৰিক ৰোগ (peripheral vascular disease), অন্ধত্ব আৰু দীৰ্ঘম্যাদী বৃক্ক ৰোগ (chronic kidney disease) হ'ব পাৰে।[2][3]
উচ্চ ৰক্তচাপক প্ৰাথমিক উচ্চ ৰক্তচাপ (Essential hypertension/primary high blood pressure) আৰু অপ্ৰধান উচ্চ ৰক্তচাপত (secondary high blood pressure) ভাগ কৰা হয়।[4] প্ৰায় ৯০-৯৫% ৰোগীৰ ক্ষেত্ৰত সেয়া প্ৰাথমিক যাক অনিৰ্দিষ্ট জীৱনশৈলী আৰু জিনীয় কাৰকৰ ববে হোৱা উচ্চ ৰক্তচাপ বোলে।[4][5] ৰোগৰ আশংকা বঢ়াব পৰা জীৱনশৈলী কাৰকৰ ভিতৰত মাত্ৰাধিক নিমখ, মেদবহুলতা, ধূমপান আৰু মদলৈ আঙুলিয়াব পাৰি।[1][4] বাকী থকা ৫-১০% ৰোগীক অপ্ৰধান উচ্চ ৰক্তচাপত অন্তৰ্ভুক্ত কৰিব পাৰি যাৰ নিৰ্দিষ্ট কাৰণ আছে। ইয়াৰ ভিতৰত দীৰ্ঘম্যাদী বৃক্ক ৰোগ, বৃক্কৰ ধমনীৰ সংকোচন, অন্তঃস্ৰাৱী ৰোগ আৰু জন্ম নিয়ন্ত্ৰক ঔষধ প্ৰধান।[4]
ৰক্তচাপক দুটা জোখেৰে বৰ্ণোৱা হয়- চিষ্ট'লিক আৰু ডায়েষ্ট'লিক চাপ। হৃদ চক্ৰ (cardiac cycle)ত এই দুটা ক্ৰমে সৰ্বোচ্চ আৰু সৰ্বনিম্ন চাপ।[1] বিশ্ৰাম অৱস্থাত শৰীৰৰ ৰক্তচাপ ১০০-১৪০ মিলিমিটাৰ পাৰা (চিষ্ট'লিক) আৰু ৬০-৯০ মিলিমিটাৰ পাৰা (ডায়েষ্ট'লিক)।[9] প্ৰাপ্তবয়স্কৰ বাবে ৰক্তচাপ অনবৰতে ১৪০/৯০ mmHgৰ বেছি থাকিলে উচ্চ ৰক্তচাপ বোলে।[4] শিশুৰ বাবে এই সংখ্যা ভিন্ন।[10] এবাৰ ৰক্তচাপ জোখাতকৈ ২৪ ঘণ্টা জুৰি জোখা ৰক্তচাপ অধিক শুদ্ধ।[8][4]
জীৱনশৈলী পৰিৱৰ্তন আৰু ঔষধে ৰক্তচাপ কমাই স্বাস্থ্যৰ গুৰুতৰ বিসংগতি ৰোধিব পাৰে।[6] জীৱনশৈলী পৰিৱৰ্তনৰ ভিতৰত ওজন কমোৱা, নিমখ কমাই খোৱা, শাৰীৰিক ব্যায়াম আৰু স্বাস্থ্যসন্মত আহাৰ গ্ৰহণ প্ৰধান।[4] এইবোৰ উপায়ে কাম নিদিলে ঔষধৰ প্ৰয়োগ কৰা হয়।[6] ৯০% মানুহৰ ক্ষেত্ৰত তিনিবিধলৈকে ঔষধে ৰক্তচাপ কমাব পাৰে।[4] বিশ্বজুৰি উচ্চ ৰক্তচাপে ১৬-৩৭% লোকৰ স্বাস্থ্যত প্ৰভাৱ পেলায়।.[4] ২০১০ চনত উচ্চ ৰক্তচাপ ১৮% মৃত্যুৰ (৯.৪ নিযুত) কাৰণ আছিল বুলি বিশ্বাস কৰা হয়।[7]
লক্ষণ আৰু চিহ্নসমূহ
উচ্চ ৰক্তচাপৰ লক্ষণ কমেইহে দেখা যায়। স্ক্ৰীনিং বা আন বেমাৰ দেখুৱাবলৈ যাওঁতেহে ৰোগনিৰ্ণয় কৰা হয়। উচ্চ ৰক্তচাপত ভোগা কোনো কোনোৱে মূৰৰ বিষ (বিশেষকৈ ৰাতিপুৱাৰ সময়ত মূৰৰ পিছফালে), মূৰ পাতল লগা, মূৰ ঘূৰোৱা, গুমগুমনিৰ নিচিনা শুনা, দেখাৰ সমস্যা বা অচেতন হোৱাৰ বৰ্ণনা দিয়ে।[11] কিন্তু এই লক্ষণবিলাক উচ্চ ৰক্তচাপৰ পৰা হোৱাতকৈ সাংসৰ্গিক উদ্বেগৰ পৰাহে হ'ব পাৰে।[12]
অপ্থাল্ম'স্ক'পেৰে পৰীক্ষা কৰোঁতে অপ্টিক ফাণ্ডাছৰ (optic fundus) সলনি দেখিবলৈ পোৱা যাব পাৰে।[13] এই সলনিবোৰক হাইপাৰ্টেন্ছিভ ৰেটিন'পেথী (hypertensive retinopathy) বোলা হয়।[13] উচ্চ ৰক্তচাপত ভোগা দিন যিমানে বাঢ়ে, ৰেটিন'পেথীৰ তীব্ৰতাও প্ৰায়েই সিমানে বাঢ়ে।[11]
অপ্ৰধান উচ্চ ৰক্তচাপ
উচ্চ ৰক্তচাপত বিশেষ লক্ষণ আৰু চিহ্ন থাকিলে সেয়া অপ্ৰধান শ্ৰেণীৰো হ'ব পাৰে অৰ্থাৎ নিৰ্দিষ্ট কাৰক থকা ৰক্তচাপ। যেনে- কুশ্বিং ছীন্দ্ৰ'মৰ (Cushing's syndrome) ফলত পেটত চৰ্বি জমা, গ্লুক'জ অসহিষ্ণুতা (glucose intolerance), চন্দ্ৰৰ দৰে মুখাবয়ব, ডিঙি/কান্ধৰ পিছফালে চৰ্বিৰ কুঁজ, আৰু পেটত ৰঙচুৱা দাগ হ'ব পাৰে।[14] হাইপাৰথাইৰইডিজমত প্ৰায়েই ভোক বঢ়াৰ লগত ওজন কমা, বেছি হৃদকম্পন, চকু ওলাই অহা (exophthalmos) আৰু হাত-ভৰিৰ কঁপনি হ;ব পাৰে। বৃক্কৰ ধমনীৰ সংকীৰ্ণতা (Renal artery stenosis)ত পেটৰ সোঁমাজৰ ওচৰত ধমনীৰ শব্দ (bruit) হ'ব পাৰে। ফিঅ'ক্ৰম'চাইট'মা (Pheochromocytoma])ত হঠাতে উচ্চ ৰক্তচাপ, মূৰৰ বিষ, বুকুৰ ধপধপনি, শেঁতা পৰা আৰু বেছিকৈ ঘমা লক্ষণ হ'ব পাৰে।ref name="ABC" />
উচ্চ ৰক্তচাপীয় সংকট
উচ্চ ৰক্তচাপ খুব বেছি হ'লে (ছিষ্ট'লিক ১৮০ বা ডায়েষ্ট'লিক ১১০ মিমি পাৰা) তাক উচ্চ ৰক্তচাপীয় সংকট (Hypertensive crisis) বোলে। অংগৰ ক্ষয়-ক্ষতি নথকা বা থকাৰ ওপৰত ভিত্তি কৰি ক্ৰমে ইয়াক উচ্চ ৰক্তচাপীয় অত্যাৱশ্যকীয়তা (hypertensive urgency) আৰু উচ্চ ৰক্তচাপীয় জৰুৰীকালীনতা বুলিব পাৰি।[15][16]
উচ্চ ৰক্তচাপীয় অত্যাৱশ্যকীয়তাত অংগৰ ক্ষয় হোৱাৰ প্ৰমাণ নাথাকে। তেতিয়া মুখেৰে খোৱা দৰবেৰে ২৪-৪৮ ঘণ্টাৰ ভিতৰত ৰক্তচাপ কমোৱা হয়।[17]
উচ্চ ৰক্তচাপীয় জৰুৰীকালীনতাত এটা বা ততোধিক অংগৰ ক্ষতি হয়।[18][19] ইৰায় ভিতৰত মগজু, বৃক্ক, হৃদয় আৰু হাওঁফাওঁ প্ৰধান। বিভ্ৰান্তি, টোপনিৰ ভাৱ, বুকুৰ বিষ আৰু উশাহ নোপোৱাৰ দৰে লক্ষণ হ'ব পাৰে।[17] এনে অৱস্থাত অংগৰ ক্ষতি ৰোধ কৰিবলৈ সোনকালে ৰক্তচাপ কমাব লাগে।[17] কিন্তু এনে কৰাৰ বাবে বিশেষ প্ৰমাণ নাই।[19]
গৰ্ভধাৰণ
প্ৰায় ৮-১০% গৰ্ভাৱস্থাত উচ্চ ৰক্তচাপে দেখা দিয়ে।[14] ছঘণ্টাৰ ব্যৱধানত দুবাৰ ৰক্তচাপ ১৪০/৯০ মিমি পাৰাৰ বেছি হ'লে গৰ্ভধাৰণৰ উচ্চ ৰক্তচাপ বোলা হয়।[20] গৰ্ভাৱস্থাৰ উচ্চ ৰক্তচাপক আগৰে পৰা থকা উচ্চ ৰক্তচাপ, প্ৰসৱাজনিত উচ্চ ৰক্তচাপ, বা প্ৰি-এক্লেম্প্চিয়াত ভাগ কৰিব পাৰি।[21]
গৰ্ভধাৰণৰ দ্বিতীয় ভাগ আৰু সন্তান প্ৰসৱৰ পাছত হোৱা গুৰুতৰ অৱস্থা প্ৰি-এক্লেম্প্চিয়াত উচ্চ ৰক্তচাপ আৰু প্ৰস্ৰাৱত প্ৰ'টিন পোৱা যায়।[14] প্ৰায় ৫% গৰ্ভাৱস্থাত হোৱা এই ৰোগত বিশ্বজুৰি প্ৰায় ১৬% মাতৃৰ মৃত্যু হয়।[14] ইয়াৰ সাধাৰণতে কোনো লক্ষণ নাথাকে আৰু নিয়মমাফিক পৰীক্ষাৰ জৰিয়তে ধৰা পৰে। কেতিয়াবা লক্ষণ থাকিলে মূৰৰ বিষ, চকুৰে ভালকৈ নেদেখা, বমি, পেটৰ বিষ আৰু হাত-ভৰি ফুলা আদিয়ে দেখা দিয়ে। প্ৰি-এক্লেম্প্চিয়াৰ চিকিৎসা নকৰিলে প্ৰাণনাশী উচ্চ ৰক্তচাপীয় সংকট এক্লেম্প্চিয়াই দেখা দিয়ে যাৰ ফলত অন্ধত্ব, মস্তিষ্ক ফুলা, কঁপনি, বৃক্কৰ ব্যৰ্থতা, DIC (তেজ গোট মৰা ৰোগ) আদি হ'ব পাৰে।[14][22]
শিশু
নৱজাতক আৰু কেঁচুৱাৰ উচ্চ ৰক্তচাপ হ'লে ওজন নবঢ়া, খিংখিঙীয়া, সপ্ৰতিভ নোহোৱা, উশাহ লোৱাৰ কষ্ট আদিয়ে দেখা দিয়ে।[23] শিশু অৱস্থাত উচ্চ ৰক্তচাপে মূৰৰ বিষ, চট্ফটনি, বেছি ভাগৰ, চকুৰে ধুঁৱলি-কুঁৱলি দেখা, নাকেৰে তেজ ওলোৱা, মুখৰ পক্ষাঘাত আদি লক্ষণ সৃষ্টি কৰে।[23][24]
কাৰক
প্ৰাথমিক উচ্চ ৰক্তচাপ
জিন আৰু পাৰিবেশিক কাৰকৰ জটিল বিনিময়ৰ ফলত উচ্চ ৰক্তচাপ হয়। ৰক্তচাপত অলপ-অচৰপ প্ৰভাৱ পেলোৱা বহু জিনীয় কাৰকৰ লগতে[25] বেছি প্ৰভাৱ পেলোৱা কিছুমান দুৰ্লভ জিনীয় কাৰকো চিনাক্ত কৰা হৈছে।[26] GWAS অধ্যয়নে ৰক্তচাপৰ লগত সম্পৰ্ক থকা ৩৫ টা জিনীয় স্থান বিচাৰি উলিয়াইছে।[27]
বয়সৰ লগে লগে ৰক্তচাপ বৃদ্ধি পায় আৰু পাছলৈ উচ্চ ৰক্তচাও হোৱা সম্ভাৱনা বাঢ়ে।[28] পাৰিবেশিক কাৰকৰ ভিতৰত নিমখ সংবেদী লোকৰ অধিক নিমখ গ্ৰহণ, ব্যায়াম নকৰা, মেদবহুলতা আৰু হতাশা আদি চিনাক্ত কৰা হৈছে।[29] অধিক কেফেইন গ্ৰহণ[30] আৰু ভিটামিন ডিৰ অভাৱৰ[31] ভূমিকা স্পষ্ট নহয়। মেদবহুলতা আৰু মেটাব'মিল ছীন্ড্ৰমত পোৱা ইন্চুলিন অৱৰোধেও উচ্চ ৰক্তচাপলৈ অৱদান আগবঢ়াব পাৰে।[32] প্ৰাৰম্ভিক ঘটনা যেনে জন্মাৱস্থাৰ কম ওজন, গৰ্ভাৱস্থাত ধূমপান আৰু স্তনপান নকৰোৱা আদিও সম্ভাব্য কাৰক হ'ব পাৰে কিন্তু এইবোৰৰ পদ্ধতি স্পষ্ট নহয়।[33] জহকালিতকৈ জাৰকালি সাধাৰণতে ৰক্তচাপে বেছি হয়।[34]
অপ্ৰধান উচ্চ ৰক্তচাপ
অপ্ৰধান উচ্চ ৰক্তচাপৰ নিৰ্দিষ্ট কাৰণ থাকে। ইয়াৰ ভিতৰত প্ৰধান হৈছে বৃক্কৰ ৰোগ।[14] আন্তঃশ্ৰাৱী ৰোগ যেনে কুশ্বিং ছীন্দ্ৰ'ম, হাইপাৰথাইৰইডিজম, হাইপ'থাইৰইডিজম, এক্ৰ'মেগেলী, ক'ন ছীন্ড্ৰ'ম, হাইপাৰপাৰাথাইৰইডিজম আৰু ফিঅ'ক্ৰম'চাইট'মাৰ ফলতো উচ্চ ৰক্তচাপ হয়।[14][35] আন কাৰকৰ ভিতৰত মেদবহুলতা, স্লীপ এপ্নিয়া, গৰ্ভধাৰণ, অত্যাধিক মদ্যপান, কিছুমান দৰব আদিলৈ আঙুলিয়াব পাৰি।[14][36] খোৱা পানীত বেছি আৰ্ছেনিক থাকিলে ৰক্তচাপ বাঢ়ে বুলি প্ৰমাণ পোৱা গৈছে।[37][38]
উচ্চ ৰক্তচাপ থকা বয়সীয়া লোকৰ Pulse pressure (ছীষ্ট'লিক আৰু ডায়েষ্ট'লিক চাপৰ ব্যৱধান) প্ৰায়েই বাঢ়ি থকা পোৱা যায়। ইয়াৰ অৰ্থ এয়েই যে ছীষ্ট'লিক চাপ অস্বাভাৱিকভাৱে বেছি, কিন্তু ডায়েষ্ট'লিক চাপ সাধাৰণ বা নিম্ন। ইয়াক "বিচ্ছিন্ন ছীষ্ট'লিক উচ্চ ৰক্তচাপ" (Isolated systolic hypertension) বোলা হয়।[39] উচ্চ ৰক্তচাপ বা বিচ্ছিন্ন ছীষ্ট'লিক উচ্চ ৰক্তচাপ থকা বয়সীয়া লোকৰ বেছি Pulse pressure-ৰ কাৰণ বয়সৰ লগে লগে বঢ়া ধমনীৰ কঠিনতা (arterial stiffness) বুলি ঠাৱৰ কৰা হৈছে।[40]
উচ্চ ৰক্তচাপৰ বেছি প্ৰান্তীয় অৱৰোধৰ কাৰণ হিচাপে কেইবাটাও প্ৰক্ৰিয়া আগবঢ়োৱা হৈছে। বৃক্কৰ লৱণ আৰু পানীৰ পৰিশোধন প্ৰক্ৰিয়াত (বিশেষকৈ renin-angiotensin system) গোলমাল হোৱাৰ প্ৰমাণ পোৱা গৈছে।[41] ছীম্পেথেকিক স্নায়ু প্ৰণালীৰো ইয়াত হাত আছে।[42] এই প্ৰক্ৰিয়াবোৰ একচেটিয়া নহয় আৰু প্ৰায়বোৰ প্ৰাথমিক উচ্চ ৰক্তচাপৰ ৰোগীত দুয়োটা প্ৰক্ৰিয়া ঘটিব পাৰে। উচ্চ ৰক্তচাপত বেছি প্ৰান্তীয় অৱৰোধ আৰু নলীকাৰ ক্ষতিৰ কাৰণ হিচাপে endothelial dysfunction আৰু নলীকাৰ প্ৰদাহকো আঙুলিয়াই দিয়া হৈছে।[43][44] উচ্চ ৰক্তচাপত ভূমিকা থকা কেইবাবিধো প্ৰতিৰক্ষা প্ৰণালীৰ ৰাসায়নিক পদাৰ্থ (immune system chemical signals) ইণ্টাৰলিউকিনৰ (interleukin) ফলত বাঢ়ে বুলি অধ্যয়নত পোৱা গৈছে।[45]
২০১৪ চনত কৰা এটা মেটা-এনালাইচিছত[46] কোৱা হৈছে যে প্ৰাপ্তবয়স্ক লোকৰ উচ্চ ৰক্তচাপত কেৱল ছ'ডিয়াম আৰু পটাছিয়ামতকৈ ছ'ডিয়াম-পটাছিয়াম অনুপাতৰ ভূমিকা অধিক।
ৰোগ নিৰ্ণয়
| প্ৰণালী | পৰীক্ষা |
|---|---|
| বৃক্ক | প্ৰস্ৰাৱৰ পৰীক্ষা, প্ৰস্ৰাৱত প্ৰ'টিন, ব্লাড-ইউৰিয়া নাইট্ৰ'জেন আৰু/বা ক্ৰিয়েটিনিন। |
| অন্তঃস্ৰাৱী | ছেৰাম ছ'ডিয়াম, পটাছিয়াম, কেল্চিয়াম, থাইৰইড ষ্টিমুলেটিং হৰম'ন |
| বিপাক | ফাষ্টিং ব্লাড গ্লুক'জ, HDL, LDL, আৰু ট'টেল ক'লেষ্টেৰল, ট্ৰাইগ্লিচাৰাইড |
| আন | হিমাট'ক্ৰিট, ই চি জি, আৰু বুকুৰ এক্স ৰে' |
| Sources: Harrison's principles of internal medicine[47] others[48][49][50][51][52] | |
Hypertension is diagnosed on the basis of a persistently high resting blood pressure. Traditionally, the National Institute of Clinical Excellence recommends three separate resting sphygmomanometer measurements at monthly intervals.[53][54] The American Heart Association recommends at least three resting measurements on at least two separate health care visits.[55] Ambulatory blood pressure monitoring over 12 to 24 hours is the most accurate method to confirm the diagnosis.[56]
An exception to this is those with very high blood pressure readings especially when there is poor organ function.[54] Initial assessment of the hypertensive people should include a complete history and physical examination. With the availability of 24-hour ambulatory blood pressure monitors and home blood pressure machines, the importance of not wrongly diagnosing those who have white coat hypertension has led to a change in protocols. In the United Kingdom, current best practice is to follow up a single raised clinic reading with ambulatory measurement, or less ideally with home blood pressure monitoring over the course of 7 days.[54] The United States Preventative Services Task Force also recommends getting measurements outside of the healthcare environment.[57] Pseudohypertension in the elderly or noncompressibility artery syndrome may also require consideration. This condition is believed to be due to calcification of the arteries resulting in abnormally high blood pressure readings with a blood pressure cuff while intra arterial measurements of blood pressure are normal.[58] Orthostatic hypertension is when blood pressure increases upon standing.[59]
Once the diagnosis of hypertension has been made, healthcare providers should attempt to identify the underlying cause based on risk factors and other symptoms, if present. Secondary hypertension is more common in preadolescent children, with most cases caused by kidney disease. Primary or essential hypertension is more common in adolescents and has multiple risk factors, including obesity and a family history of hypertension.[60] Laboratory tests can also be performed to identify possible causes of secondary hypertension, and to determine whether hypertension has caused damage to the heart, eyes, and kidneys. Additional tests for diabetes and high cholesterol levels are usually performed because these conditions are additional risk factors for the development of heart disease and may require treatment.[5]
Serum creatinine is measured to assess for the presence of kidney disease, which can be either the cause or the result of hypertension. Serum creatinine alone may overestimate glomerular filtration rate and recent guidelines advocate the use of predictive equations such as the Modification of Diet in Renal Disease (MDRD) formula to estimate glomerular filtration rate (eGFR).[61] eGFR can also provide a baseline measurement of kidney function that can be used to monitor for side effects of certain antihypertensive drugs on kidney function. Additionally, testing of urine samples for protein is used as a secondary indicator of kidney disease. Electrocardiogram (EKG/ECG) testing is done to check for evidence that the heart is under strain from high blood pressure. It may also show whether there is thickening of the heart muscle (left ventricular hypertrophy) or whether the heart has experienced a prior minor disturbance such as a silent heart attack. A chest X-ray or an echocardiogram may also be performed to look for signs of heart enlargement or damage to the heart.[14]
Adults
| Category | systolic, mm Hg | diastolic, mm Hg |
|---|---|---|
| Normal | 90–119 | 60–79 |
| High normal[9] (Prehypertension) |
120–139 | 80–89 |
| Stage 1 hypertension | 140–159 | 90–99 |
| Stage 2 hypertension | 160–179 | 100–109 |
| Stage 3 hypertension[62][63] (Hypertensive emergency) |
≥180 | ≥110 |
| Isolated systolic hypertension | ≥140 | <90 |
In people aged 18 years or older hypertension is defined as a systolic or a diastolic blood pressure measurement consistently higher than an accepted normal value (currently 139 mmHg systolic, 89 mmHg diastolic: see table – Classification (JNC7)). Lower thresholds are used (135 mmHg systolic or 85 mmHg diastolic) if measurements are derived from 24-hour ambulatory or home monitoring.[54] Recent international hypertension guidelines have also created categories below the hypertensive range to indicate a continuum of risk with higher blood pressures in the normal range. JNC7 (2003)[61] uses the term prehypertension for blood pressure in the range 120–139 mmHg systolic or 80–89 mmHg diastolic, while ESH-ESC Guidelines (2007)[62] and BHS IV (2004)[63] use optimal, normal and high normal categories to subdivide pressures below 140 mmHg systolic and 90 mmHg diastolic. Hypertension is also sub-classified: JNC7 distinguishes hypertension stage I, hypertension stage II, and isolated systolic hypertension. Isolated systolic hypertension refers to elevated systolic pressure with normal diastolic pressure and is common in the elderly.[61] The ESH-ESC Guidelines (2007)[62] and BHS IV (2004)[63] additionally define a third stage (stage III hypertension) for people with systolic blood pressure exceeding 179 mmHg or a diastolic pressure over 109 mmHg. Hypertension is classified as "resistant" if medications do not reduce blood pressure to normal levels.[61]
Children
Hypertension occurs in around 0.2 to 3% of newborns; however, blood pressure is not measured routinely in healthy newborns.[24] Hypertension is more common in high risk newborns. A variety of factors, such as gestational age, postconceptional age and birth weight needs to be taken into account when deciding if a blood pressure is normal in a newborn.[24]
Hypertension defined as elevated blood pressure over several visits affects 1% to 5% of children and adolescents and is associated with long term risks of ill-health.[64] Blood pressure rises with age in childhood and, in children, hypertension is defined as an average systolic or diastolic blood pressure on three or more occasions equal or higher than the 95th percentile appropriate for the sex, age and height of the child. High blood pressure must be confirmed on repeated visits however before characterizing a child as having hypertension.[64] Prehypertension in children has been defined as average systolic or diastolic blood pressure that is greater than or equal to the 90th percentile, but less than the 95th percentile.[64] In adolescents, it has been proposed that hypertension and pre-hypertension are diagnosed and classified using the same criteria as in adults.[64]
The value of routine screening for hypertension in children over the age of 3 years is debated.[65][66] In 2004 the National High Blood Pressure Education Program recommended that children aged 3 years and older have blood pressure measurement at least once at every health care visit[64] and the National Heart, Lung, and Blood Institute and American Academy of Pediatrics made a similar recommendation.[67] However, the American Academy of Family Physicians[68] supports the view of the U.S. preventive Services Task Force that evidence is insufficient to determine the balance of benefits and harms of screening for hypertension in children and adolescents who do not have symptoms.[69]
Prevention
Much of the disease burden of high blood pressure is experienced by people who are not labeled as hypertensive.[63] Consequently, population strategies are required to reduce the consequences of high blood pressure and reduce the need for antihypertensive drug therapy. Lifestyle changes are recommended to lower blood pressure, before starting drug therapy. The 2004 British Hypertension Society guidelines[63] proposed lifestyle changes consistent with those outlined by the US National High BP Education Program in 2002[70] for the primary prevention of hypertension:
- maintain normal body weight for adults (e.g. body mass index 20–25 kg/m2)
- reduce dietary sodium intake to <100 mmol/ day (<6 g of sodium chloride or <2.4 g of sodium per day)
- engage in regular aerobic physical activity such as brisk walking (≥30 min per day, most days of the week)
- limit alcohol consumption to no more than 3 units/day in men and no more than 2 units/day in women
- consume a diet rich in fruit and vegetables (e.g. at least five portions per day);
Effective lifestyle modification may lower blood pressure as much as an individual antihypertensive drug. Combinations of two or more lifestyle modifications can achieve even better results.[63] There is considerable evidence that reducing dietary salt intake lowers blood pressure, but whether this translates into a reduction in mortality and cardiovascular disease remains uncertain.[71] Estimated sodium intake ≥6g/day and <3g/day are both associated with high risk of death or major cardiovascular disease, but the association between high sodium intake and adverse outcomes is only observed in people with hypertension.[72] Consequently, in the absence of results from randomized controlled trials, the wisdom of reducing levels of dietary salt intake below 3g/day has been questioned.[71]
Management
According to one review published in 2003, reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34%, of ischaemic heart disease by 21%, and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease.[73]
Target blood pressure
Various expert groups have produced guidelines regarding how low the blood pressure target should be when a person is treated for hypertension. These groups recommend a target below the range 140–160 / 90–100 mmHg for the general population.[10][74][75][76][77] Controversy exists regarding the appropriate targets for certain subgroups, including the elderly, people with diabetes and people with kidney disease.[78]
Many expert groups recommend a slightly higher target of 150/90 mmHg for those over somewhere between 60 and 80 years of age.[74][75][76][79] One expert group, the JNC-8, recommends the target of 150/90 mmHg for those over 60 years of age,[10] but some experts within this group disagree with this recommendation.[80] Some expert groups have also recommended slightly lower targets in those with diabetes[74] or chronic kidney disease with proteinuria,[81] but others recommend the same target as for the general population.[10][78] The issue of what is the best target and whether targets should differ for high risk individuals is unresolved,[82] but current best evidence supports more intensive blood pressure lowering than advocated in some guidelines.[83]
Lifestyle modifications
The first line of treatment for hypertension is lifestyle changes, including dietary changes, physical exercise, and weight loss. Though these have all been recommended in scientific advisories,[84] a Cochrane systematic review found no evidence for effects of weight loss diets on death or long-term complications and adverse events in persons with hypertension.[85] The review did find a decrease in blood pressure.[85] Their potential effectiveness is similar to and at times exceeds a single medication.[9] If hypertension is high enough to justify immediate use of medications, lifestyle changes are still recommended in conjunction with medication.
Dietary changes shown to reduce blood pressure include diets with low sodium,[86][87][88] the DASH diet,[89] and vegetarian diets.[90]
Increasing dietary potassium has a potential benefit for lowering the risk of hypertension.[91][92] The 2015 Dietary Guidelines Advisory Committee (DGAC) stated that potassium is one of the shortfall nutrients which is under-consumed in the United States.[93] Potassium supplementation is challenging due to the large quantities required to achieve a substantial fraction of the 3.5 gram Daily Value [94] and the strong taste of many potassium compounds. Potassium gluconate has the mildest taste of these, but the lowest potassium content, of 16.7%.[95]
Physical exercise regimens which are shown to reduce blood pressure include isometric resistance exercise, aerobic exercise, resistance exercise, and device-guided breathing.[96]
Stress reduction techniques such as biofeedback or transcendental meditation may be considered as an add-on to other treatments to reduce hypertension, but do not have evidence for preventing cardiovascular disease on their own.[96][97][98]
Medications
Several classes of medications, collectively referred to as antihypertensive medications, are available for treating hypertension.
First line medications for hypertension include thiazide-diuretics, calcium channel blockers, angiotensin converting enzyme inhibitors and angiotensin receptor blockers.[10] These medications may be used alone or in combination; the latter option may serve to minimize counter-regulatory mechanisms that act to revert blood pressure values to pre-treatment levels.[10][99] Most people require more than one medication to control their hypertension.[84]
Resistant hypertension
Resistant hypertension is defined as hypertension that remains above goal blood pressure in spite of using, at once, three antihypertensive medications belonging to different drug classes. Low adherence to treatment is an important cause of resistant hypertension.[100] Resistant hypertension may also represent the result of chronic high activity of the autonomic nervous system; this concept is known as "neurogenic hypertension".[101]
Epidemiology


| no data <110 110-220 220-330 330-440 440-550 550-660 | 660-770 770-880 880-990 990-1100 1100-1600 >1600 |
Adults
As of 2014, approximately one billion adults or ~22% of the population of the world have hypertension.[104] It is slightly more frequent in men,[104] in those of low socioeconomic status,[5] and prevalence increases with age.[5] It is common in high, medium and low income countries.[104][105] The prevalence of raised blood pressure is highest in Africa, (30% for both sexes) and lowest in the WHO Region of the Americas (18% for both sexes). Rates also vary markedly within WHO regions with rates as low as 3.4% (men) and 6.8% (women) in rural India and as high as 68.9% (men) and 72.5% (women) in Poland.[106] In Europe hypertension occurs in about 30-45% of people as of 2013.[9] In 1995 it was estimated that 43 million people (24% of the populations) in the United States had hypertension or were taking antihypertensive medication.[107] By 2004 this had increased to 29%[108][109] and further to 34% (76 million US adults) by 2006. African American adults in the United States have among the highest rates of hypertension in the world at 44%.[110] It is also more common in Filipino Americans and less common in US whites and Mexican Americans.[5][111]
Children
Rates of high blood pressure in children and adolescents have increased in the last 20 years in the United States.[112] Childhood hypertension, particularly in pre-adolescents, is more often secondary to an underlying disorder than in adults. Kidney disease is the most common secondary cause of hypertension in children and adolescents. Nevertheless, primary or essential hypertension accounts for most cases.[113]
Outcomes
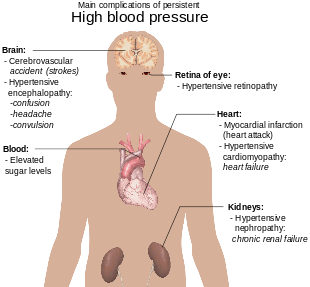
Hypertension is the most important preventable risk factor for premature death worldwide.[114] It increases the risk of ischemic heart disease[115] strokes,[14] peripheral vascular disease,[116] and other cardiovascular diseases, including heart failure, aortic aneurysms, diffuse atherosclerosis, chronic kidney disease, and pulmonary embolism.[14] Hypertension is also a risk factor for cognitive impairment and dementia.[14] Other complications include hypertensive retinopathy and hypertensive nephropathy.[61]
History
Measurement
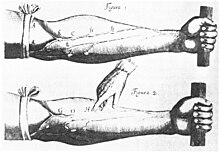
Modern understanding of the cardiovascular system began with the work of physician William Harvey (1578–1657), who described the circulation of blood in his book "De motu cordis". The English clergyman Stephen Hales made the first published measurement of blood pressure in 1733.[117][118] However, hypertension as a clinical entity came into its own with the invention of the cuff-based sphygmomanometer by Scipione Riva-Rocci in 1896.[119] This allowed easy measurement of systolic pressure in the clinic. In 1905, Nikolai Korotkoff improved the technique by describing the Korotkoff sounds that are heard when the artery is ausculated with a stethoscope while the sphygmomanometer cuff is deflated.[118] This permitted systolic and diastolic pressure to be measured.
Identification
The symptoms similar to symptoms of patients with hypertensive crisis are discussed in medieval Persian medical texts in the chapter of "fullness disease".[120] The symptoms include headache, heaviness in the head, sluggish movements, general redness and warm to touch feel of the body, prominent, distended and tense vessels, fullness of the pulse, distension of the skin, coloured and dense urine, loss of appetite, weak eyesight, impairment of thinking, yawning, drowsiness, vascular rupture, and hemorrhagic stroke.[121] Fullness disease was presumed to be due to an excessive amount of blood within the blood vessels.
Descriptions of hypertension as a disease came among others from Thomas Young in 1808 and especially Richard Bright in 1836.[117] The first report of elevated blood pressure in a person without evidence of kidney disease was made by Frederick Akbar Mahomed (1849–1884).[122]
Treatment
Historically the treatment for what was called the "hard pulse disease" consisted in reducing the quantity of blood by bloodletting or the application of leeches.[117] This was advocated by The Yellow Emperor of China, Cornelius Celsus, Galen, and Hippocrates.[117] The therapeutic approach for the treatment of hard pulse disease included changes in lifestyle (staying away from anger and sexual intercourse) and dietary program for patients (avoiding the consumption of wine, meat, and pastries, reducing the volume of food in a meal, maintaining a low-energy diet and the dietary usage of spinach and vinegar).
In the 19th and 20th centuries, before effective pharmacological treatment for hypertension became possible, three treatment modalities were used, all with numerous side-effects: strict sodium restriction (for example the rice diet[117]), sympathectomy (surgical ablation of parts of the sympathetic nervous system), and pyrogen therapy (injection of substances that caused a fever, indirectly reducing blood pressure).[117][123]
The first chemical for hypertension, sodium thiocyanate, was used in 1900 but had many side effects and was unpopular.[117] Several other agents were developed after the Second World War, the most popular and reasonably effective of which were tetramethylammonium chloride, hexamethonium, hydralazine and reserpine (derived from the medicinal plant Rauwolfia serpentina). None of these were well tolerated.[124][125] A major breakthrough was achieved with the discovery of the first well-tolerated orally available agents. The first was chlorothiazide, the first thiazide diuretic and developed from the antibiotic sulfanilamide, which became available in 1958.[117][126] Subsequently, beta blockers, calcium channel blockers, angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers and renin inhibitors were developed as antihypertensive agents.[123]
স্মাজ আৰু সংস্কৃতি
সজাগতা

[108]]]
বিশ্ব স্বাস্থ্য সংস্থাই উচ্চ ৰক্তচাপক হৃদজনিত মৃত্যুৰ মুখ্য কাৰক হিচাপে চিনাক্ত কৰিছে।[127] ৮৫ খন উচ ৰক্তচাপ ছচায়েটি আৰু লীগৰ মূল সংস্থা The World Hypertension League-এ কয় যে বিশ্বৰ উচ্চ ৰক্তচাপ থকা লোকৰ ৫০% তকৈও বেছিয়ে তেওঁলোকৰ ৰোগৰ কথা নাজানে।[127] এই সমস্যাৰ মোকাবিলা কৰিবলৈ তেওঁলোকে ২০০৫ চনত বিশ্বজুৰি এটা সজাগতা অভিযান আৰম্ভ কৰে আৰু প্ৰতি বছৰৰ ১৭ মে' তাৰিখটো বিশ্ব উচ্চ ৰক্তচাপ দিৱস হিচাপে পালন কৰে। ২০০৭ চনত ৪৭ খন দেশৰ চৰকাৰ, বেচৰকাৰী সংস্থা, ব্যক্তিগত উদ্যোগ আদিয়ে যুটীয়াভাৱে টেলিভিজন, ৰেলী আদিৰ জৰিয়তে উচ্চ ৰক্তচাপৰ সজাগতা অভিযান চলায় আৰু প্ৰায় ২৫ কোটি লোকলৈ এই বাৰ্তা যায়। WHL-এ আশা কৰে যে লাহে লাহে উচ্চ ৰক্তচাপত ভোগা প্ৰায় ১৫০ কোটি লোক ইয়াৰ প্ৰতি সজাগ হ'ব।[128]
অৰ্থনীতি
High blood pressure is the most common chronic medical problem prompting visits to primary health care providers in USA. The American Heart Association estimated the direct and indirect costs of high blood pressure in 2010 as $76.6 billion.[110] In the US 80% of people with hypertension are aware of their condition, 71% take some antihypertensive medication, but only 48% of people aware that they have hypertension adequately control it.[110]
Research
A 2015 review of several clinical studies on how vitamin D affects blood pressure showed that restoring blood vitamin D levels by using supplements (more than 1,000 IU per day) reduced blood pressure in hypertensive individuals when they had existing vitamin D deficiency.[129] The results also demonstrated a correlation of chronically low vitamin D levels with a higher chance of becoming hypertensive. Supplementation with vitamin D over 18 months in normotensive individuals with vitamin D deficiency did not significantly affect blood pressure.[129] -->
তথ্যসূত্ৰ
- ↑ 1.0 1.1 1.2 1.3 "High Blood Pressure Fact Sheet". CDC. February 19, 2015. http://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_bloodpressure.htm। আহৰণ কৰা হৈছে: 6 March 2016.
- ↑ 2.0 2.1 Lackland, DT; Weber, MA (May 2015). "Global burden of cardiovascular disease and stroke: hypertension at the core.". The Canadian journal of cardiology খণ্ড 31 (5): 569–71. doi:10.1016/j.cjca.2015.01.009. PMID 25795106.
- ↑ 3.0 3.1 Mendis, Shanthi; Puska, Pekka; Norrving, Bo (2011). Global atlas on cardiovascular disease prevention and control (1st সম্পাদনা). প্ৰকাশক Geneva: World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. পৃষ্ঠা. 38. ISBN 9789241564373. http://whqlibdoc.who.int/publications/2011/9789241564373_eng.pdf?ua=1.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 Poulter, NR; Prabhakaran, D; Caulfield, M (22 August 2015). "Hypertension.". Lancet (London, England) খণ্ড 386 (9995): 801–12. doi:10.1016/s0140-6736(14)61468-9. PMID 25832858.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Carretero OA, Oparil S; Oparil (January 2000). "Essential hypertension. Part I: definition and etiology". Circulation খণ্ড 101 (3): 329–35. doi:10.1161/01.CIR.101.3.329. PMID 10645931. http://circ.ahajournals.org/content/101/3/329.long.
- ↑ 6.0 6.1 6.2 "How Is High Blood Pressure Treated?". National Heart, Lung, and Blood Institute. September 10, 2015. http://www.nhlbi.nih.gov/health/health-topics/topics/hbp/treatment। আহৰণ কৰা হৈছে: 6 March 2016.
- ↑ 7.0 7.1 Campbell, NR; Lackland, DT; Lisheng, L; Niebylski, ML; Nilsson, PM; Zhang, XH (March 2015). "Using the Global Burden of Disease study to assist development of nation-specific fact sheets to promote prevention and control of hypertension and reduction in dietary salt: a resource from the World Hypertension League.". Journal of clinical hypertension (Greenwich, Conn.) খণ্ড 17 (3): 165–67. doi:10.1111/jch.12479. PMID 25644474.
- ↑ 8.0 8.1 Naish, Jeannette; Court, Denise Syndercombe (2014). Medical sciences (2 সম্পাদনা). পৃষ্ঠা. 562. ISBN 9780702052491. https://books.google.com/books?id=K21_AwAAQBAJ&pg=PA562.
- ↑ 9.0 9.1 9.2 9.3 Giuseppe, Mancia; Fagard, R; Narkiewicz, K; Redon, J; Zanchetti, A; Bohm, M; Christiaens, T; Cifkova, R et al. (July 2013). "2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)". European Heart Journal খণ্ড 34 (28): 2159–219. doi:10.1093/eurheartj/eht151. PMID 23771844.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 James, PA.; Oparil, S.; Carter, BL.; Cushman, WC.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, DT.; Lefevre, ML. et al. (Dec 2013). "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8)". JAMA খণ্ড 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
- ↑ 11.0 11.1 "Hypertensive vascular disease". Harrison's Principles of Internal Medicine (16th সম্পাদনা). প্ৰকাশক New York, NY: McGraw-Hill. 2005. পৃষ্ঠা. 1463–81. ISBN 0-07-139140-1.
- ↑ Marshall, IJ; Wolfe, CD; McKevitt, C (Jul 9, 2012). "Lay perspectives on hypertension and drug adherence: systematic review of qualitative research". BMJ (Clinical research ed.) খণ্ড 345: e3953. doi:10.1136/bmj.e3953. PMID 22777025.
- ↑ 13.0 13.1 Wong T, Mitchell P; Mitchell (February 2007). "The eye in hypertension". Lancet খণ্ড 369 (9559): 425–35. doi:10.1016/S0140-6736(07)60198-6. PMID 17276782.
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 14.11 O'Brien, Eoin; Beevers, D. G.; Lip, Gregory Y. H. (2007). ABC of hypertension. প্ৰকাশক London: BMJ Books. ISBN 1-4051-3061-X.
- ↑ Rodriguez, Maria Alexandra; Kumar, Siva K.; De Caro, Matthew (2010-04-01). "Hypertensive crisis". Cardiology in Review খণ্ড 18 (2): 102–07. doi:10.1097/CRD.0b013e3181c307b7. ISSN 1538-4683. PMID 20160537.
- ↑ "Hypertensive Crisis". www.heart.org. http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/AboutHighBloodPressure/Hypertensive-Crisis_UCM_301782_Article.jsp। আহৰণ কৰা হৈছে: 2015-07-25.
- ↑ 17.0 17.1 17.2 Marik PE, Varon J; Varon (June 2007). "Hypertensive crises: challenges and management". Chest খণ্ড 131 (6): 1949–62. doi:10.1378/chest.06-2490. PMID 17565029. http://chestjournal.chestpubs.org/content/131/6/1949.long.[সংযোগবিহীন উৎস]
- ↑ Chobanian, AV; Bakris, GL; Black, HR; Cushman, WC; Green, LA; Izzo JL, Jr; Jones, DW; Materson, BJ; Oparil, S; Wright JT, Jr; Roccella, EJ; Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood, Institute; National High Blood Pressure Education Program Coordinating, Committee (Dec 2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension খণ্ড 42 (6): 1206–52. doi:10.1161/01.hyp.0000107251.49515.c2. PMID 14656957.
- ↑ 19.0 19.1 Perez, MI; Musini, VM; Wright, James M (23 January 2008). "Pharmacological interventions for hypertensive emergencies.". The Cochrane database of systematic reviews (1): CD003653. doi:10.1002/14651858.CD003653.pub3. PMID 18254026.
- ↑ Harrison's principles of internal medicine. (18th সম্পাদনা). প্ৰকাশক New York: McGraw-Hill. 2011. পৃষ্ঠা. 55–61. ISBN 9780071748896.
- ↑ "Management of hypertension in pregnant and postpartum women". www.uptodate.com. http://www.uptodate.com/contents/management-of-hypertension-in-pregnant-and-postpartum-women?source=machineLearning&search=hypertension+pregnancy&selectedTitle=1~150§ionRank=1&anchor=H53704432#H53704432। আহৰণ কৰা হৈছে: 2015-07-30.
- ↑ Gibson, Paul (July 30, 2009). "Hypertension and Pregnancy". eMedicine Obstetrics and Gynecology. Medscape. http://emedicine.medscape.com/article/261435-overview। আহৰণ কৰা হৈছে: 16 June 2009.
- ↑ 23.0 23.1 Rodriguez-Cruz, Edwin; Ettinger, Leigh M (April 6, 2010). "Hypertension". eMedicine Pediatrics: Cardiac Disease and Critical Care Medicine. Medscape. http://emedicine.medscape.com/article/889877-overview। আহৰণ কৰা হৈছে: 16 June 2009.
- ↑ 24.0 24.1 24.2 Dionne JM, Abitbol CL, Flynn JT; Abitbol; Flynn (January 2012). "Hypertension in infancy: diagnosis, management and outcome". Pediatr. Nephrol. খণ্ড 27 (1): 17–32. doi:10.1007/s00467-010-1755-z. PMID 21258818.
- ↑ Ehret GB; Munroe PB; Rice KM et al. (October 2011). "Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk". Nature খণ্ড 478 (7367): 103–09. doi:10.1038/nature10405. PMID 21909115.
- ↑ Lifton, RP; Gharavi, AG, Geller, DS (2001-02-23). "Molecular mechanisms of human hypertension". Cell খণ্ড 104 (4): 545–56. doi:10.1016/S0092-8674(01)00241-0. PMID 11239411.
- ↑ Kato, Norihiro; Loh, Marie; Takeuchi, Fumihiko; Verweij, Niek; Wang, Xu; Zhang, Weihua; Kelly, Tanika N.; Saleheen, Danish et al. (2015-11-01). "Trans-ancestry genome-wide association study identifies 12 genetic loci influencing blood pressure and implicates a role for DNA methylation". Nature Genetics খণ্ড 47 (11): 1282–93. doi:10.1038/ng.3405. ISSN 1546-1718. PMID 26390057.
- ↑ Vasan, RS; Beiser, A; Seshadri, S; Larson, MG; Kannel, WB; D'Agostino, RB; Levy, D (2002-02-27). "Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study". JAMA: The Journal of the American Medical Association খণ্ড 287 (8): 1003–10. doi:10.1001/jama.287.8.1003. PMID 11866648.
- ↑ Meng, L; Chen, D; Yang, Y; Zheng, Y; Hui, R (May 2012). "Depression increases the risk of hypertension incidence: a meta-analysis of prospective cohort studies.". Journal of Hypertension খণ্ড 30 (5): 842–51. doi:10.1097/hjh.0b013e32835080b7. PMID 22343537.
- ↑ Mesas, AE; Leon-Muñoz, LM; Rodriguez-Artalejo, F; Lopez-Garcia, E (October 2011). "The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis". The American Journal of Clinical Nutrition খণ্ড 94 (4): 1113–26. doi:10.3945/ajcn.111.016667. PMID 21880846.
- ↑ Vaidya A, Forman JP; Forman (November 2010). "Vitamin D and hypertension: current evidence and future directions". Hypertension খণ্ড 56 (5): 774–79. doi:10.1161/HYPERTENSIONAHA.109.140160. PMID 20937970.
- ↑ Sorof J, Daniels S; Daniels (October 2002). "Obesity hypertension in children: a problem of epidemic proportions". Hypertension খণ্ড 40 (4): 441–47. doi:10.1161/01.HYP.0000032940.33466.12. PMID 12364344. http://hyper.ahajournals.org/cgi/pmidlookup?view=long&pmid=12364344। আহৰণ কৰা হৈছে: 3 June 2009.
- ↑ Lawlor, DA; Smith, GD (May 2005). "Early life determinants of adult blood pressure". Current Opinion in Nephrology and Hypertension খণ্ড 14 (3): 259–64. doi:10.1097/01.mnh.0000165893.13620.2b. PMID 15821420.
- ↑ Fares, A (June 2013). "Winter Hypertension: Potential mechanisms.". International journal of health sciences খণ্ড 7 (2): 210–9. doi:10.12816/0006044. PMID 24421749.
- ↑ Dluhy RG, Williams GH eds (1998). "Endocrine hypertension". Williams textbook of endocrinology (9th সম্পাদনা). প্ৰকাশক Philadelphia ; Montreal: W.B. Saunders. পৃষ্ঠা. 729–49. ISBN 0721661521.
- ↑ Grossman E, Messerli FH; Messerli (January 2012). "Drug-induced Hypertension: An Unappreciated Cause of Secondary Hypertension". Am. J. Med. খণ্ড 125 (1): 14–22. doi:10.1016/j.amjmed.2011.05.024. PMID 22195528.
- ↑ Jieying Jiangএক্সপ্ৰেছন ত্ৰুটী: অপৰিচিত শব্দ "etal" (August 2015). "Association between Arsenic Exposure from Drinking Water and Longitudinal Change in Blood Pressure among HEALS Cohort Participants". Environmental Health Perspectives খণ্ড 123 (8). doi:10.1289/ehp.1409004. PMID 25816368.
- ↑ Abhyankar, LN; Jones, MR; Guallar, E; Navas-Acien, A (April 2012). "Arsenic exposure and hypertension: a systematic review.". Environmental Health Perspectives খণ্ড 120 (4): 494–500. doi:10.1289/ehp.1103988. PMID 22138666.
- ↑ Chobanian AV (August 2007). "Clinical practice. Isolated systolic hypertension in the elderly". N. Engl. J. Med. খণ্ড 357 (8): 789–96. doi:10.1056/NEJMcp071137. PMID 17715411.
- ↑ Zieman SJ, Melenovsky V, Kass DA; Melenovsky; Kass (May 2005). "Mechanisms, pathophysiology, and therapy of arterial stiffness". Arterioscler. Thromb. Vasc. Biol. খণ্ড 25 (5): 932–43. doi:10.1161/01.ATV.0000160548.78317.29. PMID 15731494.
- ↑ Navar LG (December 2010). "Counterpoint: Activation of the intrarenal renin-angiotensin system is the dominant contributor to systemic hypertension". J. Appl. Physiol. খণ্ড 109 (6): 1998–2000; discussion 2015. doi:10.1152/japplphysiol.00182.2010a. PMID 21148349.
- ↑ Esler M, Lambert E, Schlaich M; Lambert; Schlaich (December 2010). "Point: Chronic activation of the sympathetic nervous system is the dominant contributor to systemic hypertension". J. Appl. Physiol. খণ্ড 109 (6): 1996–98; discussion 2016. doi:10.1152/japplphysiol.00182.2010. PMID 20185633.
- ↑ Versari D, Daghini E, Virdis A, Ghiadoni L, Taddei S; Daghini; Virdis; Ghiadoni; Taddei (June 2009). "Endothelium-dependent contractions and endothelial dysfunction in human hypertension". Br. J. Pharmacol. খণ্ড 157 (4): 527–36. doi:10.1111/j.1476-5381.2009.00240.x. PMID 19630832.
- ↑ Marchesi C, Paradis P, Schiffrin EL; Paradis; Schiffrin (July 2008). "Role of the renin-angiotensin system in vascular inflammation". Trends Pharmacol. Sci. খণ্ড 29 (7): 367–74. doi:10.1016/j.tips.2008.05.003. PMID 18579222.
- ↑ Gooch JL, Sharma AC; Sharma (July 2014). "Targeting the immune system to treat hypertension: where are we?". Curr Opin Nephrol Hypertens খণ্ড 23 (5): 000–000. doi:10.1097/MNH.0000000000000052. PMID 25036747.
- ↑ "Sodium-to-Potassium Ratio and Blood Pressure, Hypertension, and Related Factors". Advances in Nutrition খণ্ড 56: 712-741. 2014. PMID 25398734.
- ↑ Loscalzo, Joseph; Fauci, Anthony S.; Braunwald, Eugene; Dennis L. Kasper; Hauser, Stephen L; Longo, Dan L. (2008). Harrison's principles of internal medicine. McGraw-Hill Medical. ISBN 0-07-147691-1.
- ↑ Padwal RS; Hemmelgarn BR; Khan NA et al. (May 2009). "The 2009 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology খণ্ড 25 (5): 279–86. doi:10.1016/S0828-282X(09)70491-X. PMID 19417858.
- ↑ Padwal RJ; Hemmelgarn BR; Khan NA et al. (June 2008). "The 2008 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology খণ্ড 24 (6): 455–63. doi:10.1016/S0828-282X(08)70619-6. PMID 18548142.
- ↑ Padwal RS; Hemmelgarn BR; McAlister FA et al. (May 2007). "The 2007 Canadian Hypertension Education Program recommendations for the management of hypertension: Part 1 – blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology খণ্ড 23 (7): 529–38. doi:10.1016/S0828-282X(07)70797-3. PMID 17534459.
- ↑ Hemmelgarn BR; McAlister FA; Grover S et al. (May 2006). "The 2006 Canadian Hypertension Education Program recommendations for the management of hypertension: Part I – Blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology খণ্ড 22 (7): 573–81. doi:10.1016/S0828-282X(06)70279-3. PMID 16755312.
- ↑ Hemmelgarn BR; McAllister FA; Myers MG et al. (June 2005). "The 2005 Canadian Hypertension Education Program recommendations for the management of hypertension: part 1- blood pressure measurement, diagnosis and assessment of risk". Canadian Journal of Cardiology খণ্ড 21 (8): 645–56. PMID 16003448.
- ↑ North of England Hypertension Guideline Development Group (1 August 2004). "Frequency of measurements". Essential hypertension (NICE CG18). National Institute for Health and Clinical Excellence. পৃষ্ঠা. 53. http://www.nice.org.uk/nicemedia/pdf/CG18background.pdf। আহৰণ কৰা হৈছে: 22 December 2011.
- ↑ 54.0 54.1 54.2 54.3 National Clinical Guidance Centre (August 2011). "7 Diagnosis of Hypertension, 7.5 Link from evidence to recommendations". Hypertension (NICE CG 127). National Institute for Health and Clinical Excellence. পৃষ্ঠা. 102. http://www.nice.org.uk/nicemedia/live/13561/56007/56007.pdf। আহৰণ কৰা হৈছে: 22 December 2011.
- ↑ Aronow, WS; Fleg, JL; Pepine, CJ; Artinian, NT; Bakris, G; Brown, AS; Ferdinand, KC; Ann Forciea, M; Frishman, WH; Jaigobin, C; Kostis, JB; Mancia, G; Oparil, S; Ortiz, E; Reisin, E; Rich, MW; Schocken, DD; Weber, MA; Wesley, DJ; Harrington, RA; Bates, ER; Bhatt, DL; Bridges, CR; Eisenberg, MJ; Ferrari, VA; Fisher, JD; Gardner, TJ; Gentile, F; Gilson, MF; Hlatky, MA; Jacobs, AK; Kaul, S; Moliterno, DJ; Mukherjee, D; Rosenson, RS; Stein, JH; Weitz, HH; Wesley, DJ (Jul–Aug 2011). "ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents developed in collaboration with the American Academy of Neurology, American Geriatrics Society, American Society for Preventive Cardiology, American Society of Hypertension, American Society of Nephrology, Association of Black Cardiologists, and European Society of Hypertension". Journal of the American Society of Hypertension : JASH খণ্ড 5 (4): 259–352. doi:10.1016/j.jash.2011.06.001. PMID 21771565.
- ↑ Siu, AL (13 October 2015). "Screening for High Blood Pressure in Adults: U.S. Preventive Services Task Force Recommendation Statement.". Annals of Internal Medicine খণ্ড 163: 778–86. doi:10.7326/m15-2223. PMID 26458123.
- ↑ Siu, AL; U.S. Preventive Services Task, Force (17 November 2015). "Screening for High Blood Pressure in Adults: U.S. Preventive Services Task Force Recommendation Statement.". Annals of Internal Medicine খণ্ড 163 (10): 778–86. doi:10.7326/m15-2223. PMID 26458123.
- ↑ Franklin, SS; Wilkinson, IB; McEniery, CM (February 2012). "Unusual hypertensive phenotypes: what is their significance?". Hypertension খণ্ড 59 (2): 173–78. doi:10.1161/HYPERTENSIONAHA.111.182956. PMID 22184330.
- ↑ Kario, K (Jun 2009). "Orthostatic hypertension: a measure of blood pressure variation for predicting cardiovascular risk.". Circulation Journal খণ্ড 73 (6): 1002–07. PMID 19430163.
- ↑ Luma GB, Spiotta RT; Spiotta (May 2006). "Hypertension in children and adolescents". Am Fam Physician খণ্ড 73 (9): 1558–68. PMID 16719248.
- ↑ 61.0 61.1 61.2 61.3 61.4 61.5 Chobanian AV; Bakris GL; Black HR; Cushman WC; Green LA; Izzo Jr. JL; Jones DW; Materson BJ et al. (December 2003). "Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure". Hypertension (Joint National Committee On Prevention) খণ্ড 42 (6): 1206–52. doi:10.1161/01.HYP.0000107251.49515.c2. PMID 14656957. http://hyper.ahajournals.org/content/42/6/1206.long.
- ↑ 62.0 62.1 62.2 Mancia G; De Backer G; Dominiczak A et al. (September 2007). "2007 ESH-ESC Practice Guidelines for the Management of Arterial Hypertension: ESH-ESC Task Force on the Management of Arterial Hypertension". J. Hypertens. খণ্ড 25 (9): 1751–62. doi:10.1097/HJH.0b013e3282f0580f. PMID 17762635.
- ↑ 63.0 63.1 63.2 63.3 63.4 63.5 Williams, B; Poulter, NR, Brown, MJ, Davis, M, McInnes, GT, Potter, JF, Sever, PS, McG Thom, S, British Hypertension, Society (March 2004). "Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV". Journal of Human Hypertension খণ্ড 18 (3): 139–85. doi:10.1038/sj.jhh.1001683. PMID 14973512.
- ↑ 64.0 64.1 64.2 64.3 64.4 National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (August 2004). "The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents". Pediatrics খণ্ড 114 (2 Suppl 4th Report): 555–76. doi:10.1542/peds.114.2.S2.555. PMID 15286277.
- ↑ Chiolero, A; Bovet, P; Paradis, G (Mar 1, 2013). "Screening for elevated blood pressure in children and adolescents: a critical appraisal.". JAMA pediatrics খণ্ড 167 (3): 266–73. doi:10.1001/jamapediatrics.2013.438. PMID 23303490.
- ↑ Daniels, SR.; Gidding, SS. (Mar 2013). "Blood pressure screening in children and adolescents: is the glass half empty or more than half full?". JAMA Pediatr খণ্ড 167 (3): 302–04. doi:10.1001/jamapediatrics.2013.439. PMID 23303514.
- ↑ Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute (Dec 2011). "Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report". Pediatrics খণ্ড 128 Suppl 5: S213–56. doi:10.1542/peds.2009-2107C. PMID 22084329.
- ↑ http://www.aafp.org/patient-care/clinical-recommendations/all/hypertension.html
- ↑ Moyer, VA.; U.S. Preventive Services Task Force (October 2013). "Screening for Primary Hypertension in Children and Adolescents: U.S. Preventive Services Task Force Recommendation Statement*". Annals of Internal Medicine খণ্ড 159 (9): 613–19. doi:10.7326/0003-4819-159-9-201311050-00725. PMID 24097285.
- ↑ Whelton PK et al. (2002). "Primary prevention of hypertension. Clinical and public health advisory from the National High Blood Pressure Education Program". JAMA খণ্ড 288 (15): 1882–88. doi:10.1001/jama.288.15.1882. PMID 12377087.
- ↑ 71.0 71.1 "Evidence-based policy for salt reduction is needed". Lancet খণ্ড 388 (10043): 438. 30 July 2016. doi:10.1016/S0140-6736(16)31205-3. PMID 27507743.
- ↑ Mente, Andrew; O'Donnell, Martin; Rangarajan, Sumathy; Dagenais, Gilles; Lear, Scott; McQueen, Matthew; Diaz, Rafael; Avezum, Alvaro et al. (July 2016). "Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies". The Lancet খণ্ড 388 (10043): 465–75. doi:10.1016/S0140-6736(16)30467-6. PMID 27216139.
- ↑ Law M, Wald N, Morris J; Wald; Morris (2003). "Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy". Health Technol Assess খণ্ড 7 (31): 1–94. doi:10.3310/hta7310. PMID 14604498. Archived from the original on 4 March 2011. https://web.archive.org/web/20110304150457/http://www.hta.ac.uk/fullmono/mon731.pdf.
- ↑ 74.0 74.1 74.2 Members, Authors/Task Force; Mancia, Giuseppe; Fagard, Robert; Narkiewicz, Krzysztof; Redon, Josep; Zanchetti, Alberto; Böhm, Michael; Christiaens, Thierry et al. (2013-06-13). "2013 ESH/ESC Guidelines for the management of arterial hypertension". European Heart Journal খণ্ড 34: eht151. doi:10.1093/eurheartj/eht151. ISSN 0195-668X. PMID 23771844. http://eurheartj.oxfordjournals.org/content/early/2013/06/13/eurheartj.eht151.
- ↑ 75.0 75.1 Daskalopoulou, Stella S.; Rabi, Doreen M.; Zarnke, Kelly B.; Dasgupta, Kaberi; Nerenberg, Kara; Cloutier, Lyne; Gelfer, Mark; Lamarre-Cliche, Maxime et al. (2015-01-01). "The 2015 Canadian Hypertension Education Program Recommendations for Blood Pressure Measurement, Diagnosis, Assessment of Risk, Prevention, and Treatment of Hypertension". Canadian Journal of Cardiology খণ্ড 31 (5): 549–68. doi:10.1016/j.cjca.2015.02.016. http://dx.doi.org/10.1016/j.cjca.2015.02.016.
- ↑ 76.0 76.1 "Hypertension | 1-recommendations | Guidance and guidelines | NICE". www.nice.org.uk. Retrieved 2015-08-04.
- ↑ Arguedas, JA; Perez, MI; Wright, JM (8 July 2009). "Treatment blood pressure targets for hypertension.". The Cochrane database of systematic reviews (3): CD004349. doi:10.1002/14651858.CD004349.pub2. PMID 19588353.
- ↑ 78.0 78.1 Arguedas, JA; Leiva, V; Wright, JM (Oct 30, 2013). "Blood pressure targets for hypertension in people with diabetes mellitus.". The Cochrane database of systematic reviews খণ্ড 10: CD008277. doi:10.1002/14651858.cd008277.pub2. PMID 24170669.
- ↑ "Pharmacologic Treatment of Hypertension in Adults Aged 60 Years or Older to Higher Versus Lower Blood Pressure Targets: A Clinical Practice Guideline From the American College of Physicians and the American Academy of Family Physicians". Annals of Internal Medicine খণ্ড 166: 430. 17 January 2017. doi:10.7326/M16-1785.
- ↑ Wright JT, Jr; Fine, LJ; Lackland, DT; Ogedegbe, G; Dennison Himmelfarb, CR (1 April 2014). "Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view.". Annals of Internal Medicine খণ্ড 160 (7): 499–503. doi:10.7326/m13-2981. PMID 24424788.
- ↑ "KDIGO Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease". Kidney International Supplement. December 2012. http://www.kdigo.org/clinical_practice_guidelines/pdf/KDIGO_BP_GL.pdf.
- ↑ Brunström, Mattias; Carlberg, Bo (2016-01-30). "Lower blood pressure targets: to whom do they apply?". Lancet (London, England) খণ্ড 387 (10017): 405–06. doi:10.1016/S0140-6736(15)00816-8. ISSN 1474-547X. PMID 26559745.
- ↑ Xie, Xinfang; Atkins, Emily; Lv, Jicheng; Rodgers, Anthony (2016-06-10). "Intensive blood pressure lowering – Authors' reply". The Lancet খণ্ড 387 (10035): 2291. doi:10.1016/S0140-6736(16)30366-X. PMID 27302266. http://www.sciencedirect.com/science/article/pii/S014067361630366X.
- ↑ 84.0 84.1 Go, AS; Bauman, M; King, SM; Fonarow, GC; Lawrence, W; Williams, KA; Sanchez, E (Nov 15, 2013). "An Effective Approach to High Blood Pressure Control: A Science Advisory From the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention". Hypertension খণ্ড 63 (4): 878–85. doi:10.1161/HYP.0000000000000003. PMID 24243703. http://hyper.ahajournals.org/content/early/2013/11/14/HYP.0000000000000003.
- ↑ 85.0 85.1 Semlitsch, T; Jeitler, K; Berghold, A; Horvath, K; Posch, N; Poggenburg, S; Siebenhofer, A (2 March 2016). "Long-term effects of weight-reducing diets in people with hypertension.". The Cochrane database of systematic reviews খণ্ড 3: CD008274. doi:10.1002/14651858.CD008274.pub3. PMID 26934541. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD008274.pub3/abstract। আহৰণ কৰা হৈছে: 9 March 2016.
- ↑ "Effect of lower sodium intake on health: systematic review and meta-analyses.". BMJ খণ্ড 346: f1326. 2013. doi:10.1136/bmj.f1326. PMID 23558163.
- ↑ He, FJ; Li, J; Macgregor, GA (April 2013). "Effect of longer-term modest salt reduction on blood pressure". Cochrane Database of Systematic Reviews খণ্ড 30 (4): CD004937. doi:10.1002/14651858.CD004937.pub2. PMID 23633321.
- ↑ Karppanen, Heikki; Mervaala, Eero (2006-10-01). "Sodium intake and hypertension". Progress in Cardiovascular Diseases খণ্ড 49 (2): 59–75. doi:10.1016/j.pcad.2006.07.001. ISSN 0033-0620. PMID 17046432.
- ↑ Sacks, F. M.; Svetkey, L. P.; Vollmer, W. M.; Appel, L. J.; Bray, G. A.; Harsha, D.; Obarzanek, E.; Conlin, P. R. et al. (2001-01-04). "Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group". The New England Journal of Medicine খণ্ড 344 (1): 3–10. doi:10.1056/NEJM200101043440101. ISSN 0028-4793. PMID 11136953.
- ↑ Yokoyama, Yoko; Nishimura, Kunihiro; Barnard, Neal D.; Takegami, Misa; Watanabe, Makoto; Sekikawa, Akira; Okamura, Tomonori; Miyamoto, Yoshihiro (2014). "Vegetarian Diets and Blood Pressure". JAMA Internal Medicine খণ্ড 174 (4): 577–87. doi:10.1001/jamainternmed.2013.14547. ISSN 2168-6106. PMID 24566947.
- ↑ Aburto, NJ; Hanson, S; Gutierrez, H; Hooper, L; Elliott, P; Cappuccio, FP (3 April 2013). "Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses.". BMJ (Clinical research ed.) খণ্ড 346: f1378. doi:10.1136/bmj.f1378. PMID 23558164.
- ↑ Stone, MS; Martyn, L; Weaver, CM (22 July 2016). "Potassium Intake, Bioavailability, Hypertension, and Glucose Control.". Nutrients খণ্ড 8 (7): 444. doi:10.3390/nu8070444. PMID 27455317.
- ↑ "Scientific Report of the 2015 Dietary Guidelines Advisory Committee". https://health.gov/dietaryguidelines/2015-scientific-report/। আহৰণ কৰা হৈছে: 2017-04-26.
- ↑ "U.S. Department of Health & Human Services, National Institutes of Health, Office of Dietary Supplements, Daily Values". https://ods.od.nih.gov/HealthInformation/dailyvalues.aspx। আহৰণ কৰা হৈছে: 2017-04-25.
- ↑ "Food Business News article: Potassium: promising yet problematic". http://www.foodbusinessnews.net/articles/news_home/Supplier-Innovations/2015/01/Potassium_promising_yet_proble.aspx?ID=%7BEFE46B8B-5647-4150-9525-F66F794BF84C%7D। আহৰণ কৰা হৈছে: 2017-04-25.
- ↑ 96.0 96.1 Brook, RD; Appel, LJ; Rubenfire, M; Ogedegbe, G; Bisognano, JD; Elliott, WJ; Fuchs, FD; Hughes, JW; Lackland, DT; Staffileno, BA; Townsend, RR; Rajagopalan, S; American Heart Association Professional Education Committee of the Council for High Blood Pressure Research, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, and Council on Nutrition, Physical, Activity (Jun 2013). "Beyond medications and diet: alternative approaches to lowering blood pressure: a scientific statement from the American Heart Association". Hypertension খণ্ড 61 (6): 1360–83. doi:10.1161/HYP.0b013e318293645f. PMID 23608661.
- ↑ Nagele, Eva; Jeitler, Klaus; Horvath, Karl; Semlitsch, Thomas; Posch, Nicole; Herrmann, Kirsten H.; Grouven, Ulrich; Hermanns, Tatjana et al. (2014). "Clinical effectiveness of stress-reduction techniques in patients with hypertension". Journal of Hypertension খণ্ড 32 (10): 1936–44. doi:10.1097/HJH.0000000000000298. ISSN 0263-6352. PMID 25084308.
- ↑ Dickinson, HO; Campbell, F; Beyer, FR; Nicolson, DJ; Cook, JV; Ford, GA; Mason, JM (23 January 2008). "Relaxation therapies for the management of primary hypertension in adults.". The Cochrane database of systematic reviews (1): CD004935. doi:10.1002/14651858.CD004935.pub2. PMID 18254065.
- ↑ Chen, JM; Heran, BS; Wright, JM (7 October 2009). "Blood pressure lowering efficacy of diuretics as second-line therapy for primary hypertension.". The Cochrane database of systematic reviews (4): CD007187. doi:10.1002/14651858.CD007187.pub2. PMID 19821398.
- ↑ Santschi, V; Chiolero, A; Burnier, M (Nov 2009). "Electronic monitors of drug adherence: tools to make rational therapeutic decisions.". Journal of Hypertension খণ্ড 27 (11): 2294–95; author reply 2295. doi:10.1097/hjh.0b013e328332a501. PMID 20724871.
- ↑ Zubcevic J, Waki H, Raizada MK, Paton JF; Waki; Raizada; Paton (June 2011). "Autonomic-immune-vascular interaction: an emerging concept for neurogenic hypertension". Hypertension খণ্ড 57 (6): 1026–33. doi:10.1161/HYPERTENSIONAHA.111.169748. PMID 21536990. PMC 3105900. http://hyper.ahajournals.org/content/57/6/1026.long.
- ↑ "Blood Pressure". World Health Organization. http://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence/en/। আহৰণ কৰা হৈছে: 22 April 2017.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. http://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html। আহৰণ কৰা হৈছে: 11 November 2009.
- ↑ 104.0 104.1 104.2 "Raised blood pressure". World Health Organization. Global Health Observatory (GHO) data. http://www.who.int/gho/ncd/risk_factors/blood_pressure_text/en/.
- ↑ Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J; Whelton; Reynolds; Muntner; Whelton; He (2005). "Global burden of hypertension: analysis of worldwide data". Lancet খণ্ড 365 (9455): 217–23. doi:10.1016/S0140-6736(05)17741-1. PMID 15652604.
- ↑ Kearney PM, Whelton M, Reynolds K, Whelton PK, He J; Whelton; Reynolds; Whelton; He (January 2004). "Worldwide prevalence of hypertension: a systematic review". J. Hypertens. খণ্ড 22 (1): 11–9. doi:10.1097/00004872-200401000-00003. PMID 15106785.
- ↑ Burt VL; Whelton P; Roccella EJ et al. (March 1995). "Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991". Hypertension খণ্ড 25 (3): 305–13. doi:10.1161/01.HYP.25.3.305. PMID 7875754. http://hyper.ahajournals.org/cgi/pmidlookup?view=long&pmid=7875754। আহৰণ কৰা হৈছে: 5 June 2009.
- ↑ 108.0 108.1 Burt VL; Cutler JA; Higgins M et al. (July 1995). "Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991". Hypertension খণ্ড 26 (1): 60–69. doi:10.1161/01.HYP.26.1.60. PMID 7607734. http://hyper.ahajournals.org/cgi/pmidlookup?view=long&pmid=7607734। আহৰণ কৰা হৈছে: 5 June 2009.
- ↑ Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S; Dillon; Hughes; Carroll; Yoon (July 2007). "Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004". Journal of the American Geriatrics Society খণ্ড 55 (7): 1056–65. doi:10.1111/j.1532-5415.2007.01215.x. PMID 17608879.
- ↑ 110.0 110.1 110.2 Lloyd-Jones D; Adams RJ; Brown TM et al. (February 2010). "Heart disease and stroke statistics--2010 update: a report from the American Heart Association". Circulation খণ্ড 121 (7): e46–e215. doi:10.1161/CIRCULATIONAHA.109.192667. PMID 20019324.
- ↑ "Culture-Specific of Health Risk Health Status: Morbidity and Mortality". Stanford. https://geriatrics.stanford.edu/ethnomed/filipino/health_risk_patterns.html। আহৰণ কৰা হৈছে: 12 April 2016.
- ↑ Falkner B (May 2009). "Hypertension in children and adolesents: epidemiology and natural history". Pediatr. Nephrol. খণ্ড 25 (7): 1219–24. doi:10.1007/s00467-009-1200-3. PMID 19421783.
- ↑ Luma GB, Spiotta RT; Spiotta (May 2006). "Hypertension in children and adolescents". Am Fam Physician খণ্ড 73 (9): 1558–68. PMID 16719248. http://www.aafp.org/afp/20060501/1558.html.
- ↑ "Global health risks: mortality and burden of disease attributable to selected major risks". World Health Organization. 2009. http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf। আহৰণ কৰা হৈছে: 10 February 2012.
- ↑ Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Clarke; Qizilbash; Peto; Collins; Prospective Studies (December 2002). "Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies". Lancet খণ্ড 360 (9349): 1903–13. doi:10.1016/S0140-6736(02)11911-8. PMID 12493255.
- ↑ Singer DR, Kite A; Kite (June 2008). "Management of hypertension in peripheral arterial disease: does the choice of drugs matter?". European Journal of Vascular and Endovascular Surgery খণ্ড 35 (6): 701–08. doi:10.1016/j.ejvs.2008.01.007. PMID 18375152.
- ↑ 117.0 117.1 117.2 117.3 117.4 117.5 117.6 117.7 Esunge PM (October 1991). "From blood pressure to hypertension: the history of research". J R Soc Med খণ্ড 84 (10): 621. PMID 1744849.
- ↑ 118.0 118.1 Kotchen TA (October 2011). "Historical trends and milestones in hypertension research: a model of the process of translational research". Hypertension খণ্ড 58 (4): 522–38. doi:10.1161/HYPERTENSIONAHA.111.177766. PMID 21859967.
- ↑ Postel-Vinay N, ed (1996). A century of arterial hypertension 1896–1996. প্ৰকাশক Chichester: Wiley. পৃষ্ঠা. 213. ISBN 0-471-96788-2.
- ↑ "The medieval origins of the concept of hypertension". Heart Views খণ্ড 15 (3): 96–98. 2014. doi:10.4103/1995-705X.144807. http://www.heartviews.org/article.asp?issn=1995-705X;year=2014;volume=15;issue=3;spage=96;epage=98;aulast=Heydari। আহৰণ কৰা হৈছে: 25 November 2014.
- ↑ Emtiazy M, Choopani R, Khodadoost M, Tansaz M, Dehghan S, Ghahremani Z (2014). "Avicenna's doctrine about arterial hypertension.". Acta Med Hist Adriat খণ্ড 12: 157–62. PMID 25310615.
- ↑ Swales JD, ed (1995). Manual of hypertension. প্ৰকাশক Oxford: Blackwell Science. পৃষ্ঠা. xiii. ISBN 0-86542-861-1.
- ↑ 123.0 123.1 Dustan HP, Roccella EJ, Garrison HH; Roccella; Garrison (September 1996). "Controlling hypertension. A research success story". Arch. Intern. Med. খণ্ড 156 (17): 1926–35. doi:10.1001/archinte.156.17.1926. PMID 8823146.
- ↑ Lyons, RH; Hoobler, SW; Neligh, RB; Moe, GK; Peet, MM (1948-02-28). "Experiences with tetraethylammonium chloride in hypertension". JAMA খণ্ড 136 (9): 608–13. doi:10.1001/jama.1948.02890260016005. ISSN 0002-9955. http://dx.doi.org/10.1001/jama.1948.02890260016005.
- ↑ Bakris, G. L.; Frohlich, E. D. (1989-12-01). "The evolution of antihypertensive therapy: an overview of four decades of experience". Journal of the American College of Cardiology খণ্ড 14 (7): 1595–608. doi:10.1016/0735-1097(89)90002-8. ISSN 0735-1097. PMID 2685075.
- ↑ Novello FC, Sprague JM; Sprague (1957). "Benzothiadiazine dioxides as novel diuretics". J. Am. Chem. Soc. খণ্ড 79 (8): 2028–29. doi:10.1021/ja01565a079.
- ↑ 127.0 127.1 Chockalingam A (May 2007). "Impact of World Hypertension Day". Canadian Journal of Cardiology খণ্ড 23 (7): 517–19. doi:10.1016/S0828-282X(07)70795-X. PMID 17534457.
- ↑ Chockalingam A (June 2008). "World Hypertension Day and global awareness". Canadian Journal of Cardiology খণ্ড 24 (6): 441–44. doi:10.1016/S0828-282X(08)70617-2. PMID 18548140.
- ↑ 129.0 129.1 Chen, S; Sun, Y; Agrawal, DK (2015). "Vitamin D deficiency and essential hypertension.". Journal of the American Society of Hypertension খণ্ড 9 (11): 885–901. doi:10.1016/j.jash.2015.08.009. PMID 26419755.
অতিৰিক্ত পঠন
- James, Paul A.; Oparil, Suzanne; Carter, Barry L.; Cushman, William C.; Dennison-Himmelfarb, Cheryl; Handler, Joel; Lackland, Daniel T.; Lefevre, Michael L. et al. (18 December 2013). "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults". JAMA খণ্ড 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
বাহ্যিক সংযোগ
| বৰ্গীকৰণ | |
|---|---|
| বাহ্যিক সমল |
| ৱিকিমিডিয়া কমন্সত Hypertension সম্পৰ্কীয় মিডিয়া ফাইল আছে। |
![]() traveling with high blood pressure ভ্ৰমণ নিৰ্দেশিকা, ৱিকিভয়াজৰ পৰা
traveling with high blood pressure ভ্ৰমণ নিৰ্দেশিকা, ৱিকিভয়াজৰ পৰা
- উচ্চ ৰক্তচাপ বিষয়ে Curlie (DMOZ)-ত থকা তথ্য
